The Follow-Up Care Checklist for Myopia Management is crafted to ensure comprehensive monitoring of myopia treatment progress and facilitate necessary adjustments. By systematically assessing key indicators such as visual acuity, axial length (AL), and patient feedback, practitioners can maintain an effective and responsive myopia management plan. Pair this checklist with the Comprehensive Myopia Assessment Exam Template for a structured approach to recording and evaluating patient data.
STEP 1: Review Patient History and Current Treatment
- Previous Visit Summary:
- Date of Last Appointment: Record the date of the previous visit to track the time elapsed since the last evaluation.
- Current Treatment Plan: Document the treatment plan implemented during the last visit.
- Treatment Adherence:
- Patient Compliance: Evaluate how well the patient has adhered to the prescribed treatment regimen (e.g. number of hours of lens wear per day, missed doses of medication, etc.)
- Issues with Treatment Compliance: Identify any problems or barriers affecting adherence to the treatment plan.
- Adverse Reactions (e.g., discomfort with lenses, sensitivity to light): Identify any negative reactions to medications or lenses that could affect adherence to treatment.
- Impact on Daily Activities: Assess if the treatment prescribed has had any undesirable effects on the patient’s daily life or comfort.
- Download the Treatment Adherence Questionnaire to streamline this evaluation.
- Review of Visual Symptoms:
- Blurry Vision: Document any complaint of visual changes that could indicate a refractive shift.
- Eye Strain: Note any reports of eye strain or discomfort that could indicate issues with treatment.
- Headaches: Record any occurrences of headaches, which might be related to changes in visual correction.
- Other: Include any additional visual symptoms reported by the patient.
- Review of Lifestyle Factors:
- Changes in Outdoor Activity Time: Note any reductions in time spent outdoors per day, as this can influence myopia development.
- Increased Time Spent on Near Work: Assess if there has been a significant increase in sustained near work per day, which may impact myopia progression.
- Alterations in Screen Time: Record any changes in digital screen time.
- Other Relevant Lifestyle Changes: Include any other lifestyle changes that could impact myopia management.
STEP 2: Assess Treatment Efficacy
Routine Examination
- Visual Acuity Testing: Compare current distance and near visual acuity with previous measurements to evaluate treatment impact.
- Refraction Testing:
- Subjective Refraction: Conducted to monitor shifts in refractive error and adjust prescriptions as needed. Note that results can vary for patients using orthokeratology lenses based on lens wear compliance, such as the number of hours the lenses are worn overnight.
- Over-Refraction: Performed over existing contact lenses, such as soft multifocal lenses, to identify and correct any remaining refractive errors, allowing for precise adjustments.
- Axial Length Measurement: Regular monitoring of axial length every 6 months provides precise data on the eye’s elongation, which is key to tracking myopia progression. This practice not only aids in evaluating treatment efficacy but also helps identify the risk of complications associated with increased axial length. By plotting these measurements on a trend graph, such as the MYAH® RX/AL Trends plot, you can easily visualize changes over time. Tracking AL is particularly helpful when subjective refraction data may be inconsistent, such as in ortho-K patients who may not wear lenses consistently. Typically, an annual increase of around 0.1 mm is linked with normal eye development, while an increase of 0.2 to 0.3 mm per year may indicate worsening myopia. However, this can vary based on factors such as age, gender, race, and baseline axial length.
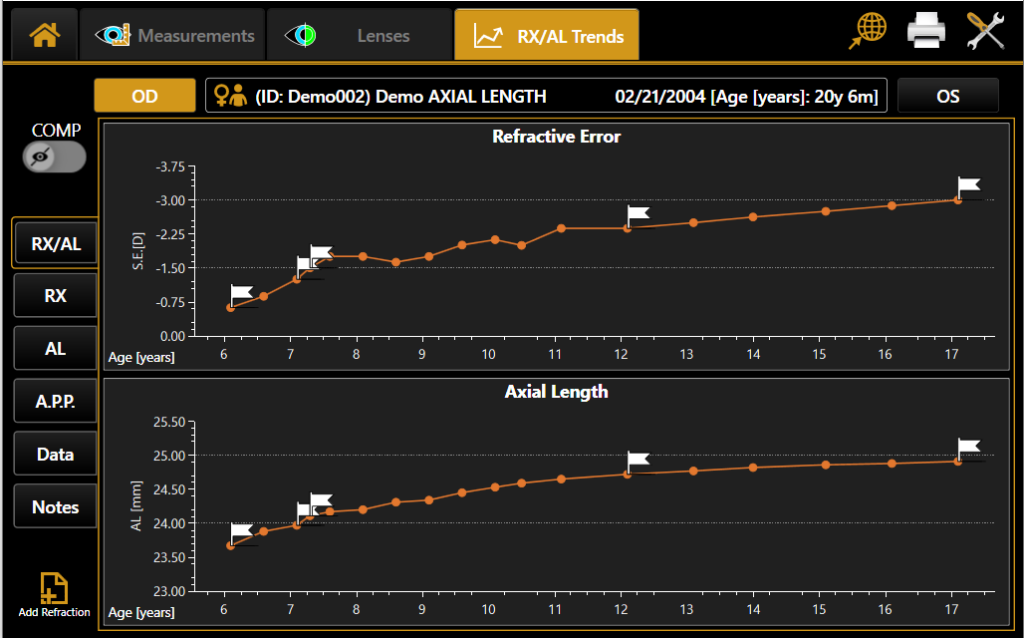
MYAH RX/AL Trends Graph (Automatically Generated from Visit-to-Visit)
- Binocular Vision Assessment: Studies have suggested that treatments such as atropine, multifocal contact lenses, and orthokeratology can impact accommodative and binocular function. Therefore, it is important to monitor any changes in key aspects, including the amplitude of accommodation, accuracy, and facility of accommodation, distance and near heterophorias, near fixation disparity, and the accommodative convergence/accommodation (AC/A) ratio.
- Slit lamp evaluation: Slit lamp evaluation is a key part of regular follow-up visits for monitoring ocular health. It is vital for assessing the fit and condition of orthokeratology lenses, ensuring they are properly aligned and free from debris or damage that could affect treatment effectiveness and patient comfort. Additionally, a detailed examination of the cornea helps in the early detection of potential complications related to contact lens wear, such as corneal edema, neovascularization, or infection. This thorough evaluation enables timely adjustments to treatment and supports overall eye health.
If Indicated (Frequency and Treatment Dependent)
- Objective (Cycloplegic) Refraction: Cycloplegic refraction allows for an accurate assessment of true refractive shifts compared to baseline. This can be valuable for troubleshooting and helping determine whether changes in visual acuity are due to true shifts in refractive error or temporary fluctuations.
- Corneal Topography: For patients using orthokeratology lenses, repeating corneal topography evaluates changes in corneal shape and curvature due to lens wear, ensuring optimal fit and treatment effectiveness. It also aids in assessing the size and centration of the treatment zone, troubleshooting potential visual complaints, and customizing and refining the lens to enhance overall treatment efficacy and patient satisfaction.
- Pupil Examination: Regular pupillometry facilitates the customization of treatment plans by enabling adjustments to orthokeratology (Ortho-K) lens designs or fine-tuning atropine dosages based on clinical data, ensuring optimal treatment efficacy and patient satisfaction. For Ortho-K, measuring pupil size and position can be used to assess the alignment of the treatment zone of the lenses with respect to the pupil, which may impact the degree of myopia control. In atropine therapy, tracking pupil responses is useful for identifying side effects such as mydriasis, which can affect amplitude of accommodation and impact near-vision tasks.
- Dry Eye Evaluation: With increasing evidence of dry eye impacting younger populations, particularly due to frequent digital device use, incorporating regular dry eye evaluations into both baseline and follow-up assessments is vital. Dry eye symptoms can arise or be exacerbated by myopia management interventions. Contact lens wear is a known factor that can contribute to dry eye and discomfort, potentially leading to lens dropout. Additionally, some atropine formulations contain preservatives like benzalkonium chloride (BAK), which can harm the ocular surface and cause dry eye with long-term use. Regular evaluations using tests like tear break-up time (TBUT) and meibomian gland imaging can be helpful for the early detection and effective management of dry eye and meibomian gland dysfunction to optimize patient comfort and treatment outcomes.
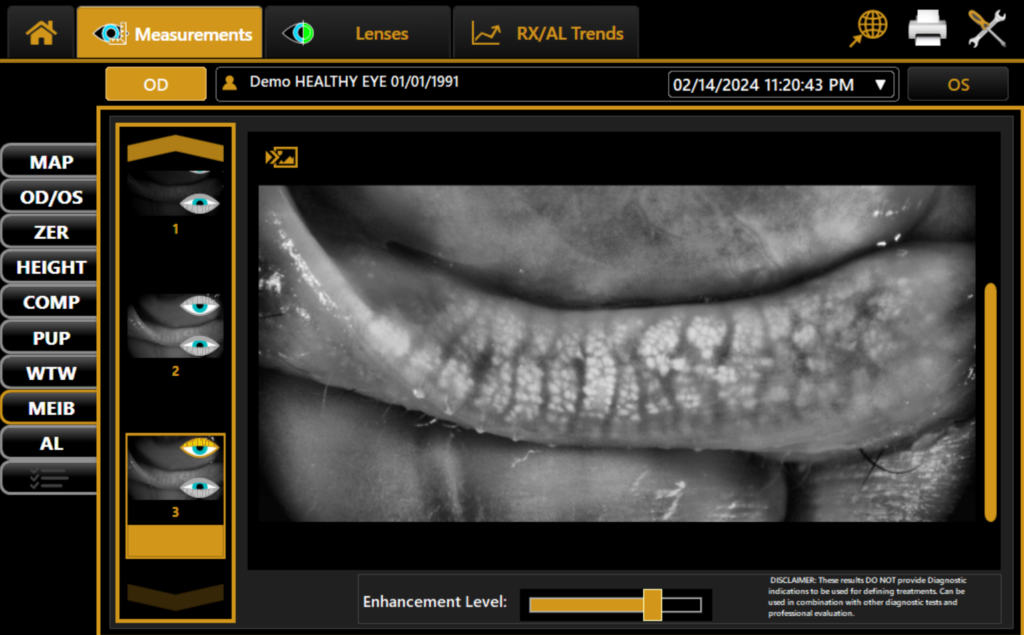
Meibomian Gland Imaging Captured with MYAH
- Retinal Health Assessment: Routine dilated fundus examination is essential for detecting retinal changes such as chorioretinal atrophy, staphyloma, and peripapillary atrophy. Particularly for high myopes (>5.00 to 6.00D), this should be performed annually due to their increased risk of retinal detachments, myopic maculopathy, and glaucoma. Optical Coherence Tomography (OCT) and fundus photography are crucial for objectively documenting retinal features, monitoring changes, and applying grading and scaling to track disease progression.
STEP 3: Update Treatment Plan
- Evaluate Treatment Outcomes:
- Changes in Myopia Severity: Asses the amount of myopia progression based on refractive error and axial length changes.
- Patient Feedback: Take into consideration the patient’s feedback regarding compliance, lifestyle impact, and any complaints to assess the appropriateness of the current treatment
- Update Treatment Plan:
- Revise Recommendations: Adjust the treatment plan as needed based on the patient feedback and examination findings. Update prescriptions as necessary to enhance treatment efficacy.
- Schedule Additional Testing: Arrange further testing if required to refine the treatment approach (e.g. cycloplegic refraction).
- Schedule Follow-Up Appointments:
- Set Next Appointment Date: Regular follow-up visits are essential for maintaining effective treatment and addressing any changes in the patient’s condition. Schedule the next appointment to monitor progress and make any necessary adjustments. Typically, scheduling appointments every six months is recommended, but the frequency may vary based on individual needs. If significant myopia progression is observed, consider more frequent visits for closer monitoring and timely intervention. Emphasize to parents that managing myopia is a long-term commitment, requiring ongoing monitoring and adjustments to achieve optimal results.
- Reference the Follow-Up Protocol Checklist to assist in scheduling future appointments and to review a breakdown of recommended assessments to be conducted during each visit.
- Patient Education:
- Review Updated Management Plan: Explain any changes in the treatment plan to the patient, ensuring they understand the updates and the reasons behind them.
- Provide Instructions on New Treatment: Give clear and detailed guidance on any new or modified treatments, including how and when to use them.
- Repeat Advice: Continue to offer guidance on lifestyle adjustments and the importance of ongoing monitoring to support treatment goals.
This detailed checklist ensures a thorough review of the patient’s progress, effective treatment evaluation, and appropriate adjustments to manage myopia effectively.



